Varicose veins of the lower extremities are rightly considered the most common pathology of peripheral vessels, it is one of the top ten so-called civilizational diseases. According to epidemiological studies, venous insufficiency occurs in 80% of people of working age. In most cases, varicose veins of the legs do not cause serious suffering, and sometimes go unnoticed at all, do not require any treatment. However, there are situations in which it is worth, without delay, to consult a specialist, to undergo appropriate therapy. What are the treatments for varicose veins of the lower extremities? What are their advantages and disadvantages?
Ways to get rid of the disease
Thousands of people a year wonder: how to get rid of "ugly knots" or "vascular networks" on their feet? Media portals are full of ads for public and private clinics that treat varicose veins of the lower extremities. They offer "unique, " "guaranteed, " "painless, " or "completely safe" ways to get rid of this ailment. Sometimes it is difficult to understand this advertisement, to answer the question of which treatment option is the most appropriate. If a person has decided to deal with their dilated blood vessels and is unsure of the safety or effectiveness of this or that method of treatment, the best option for him is to contact several clinics to get qualified advice from at least two experts.
There are various reasons why a patient with varicose veins should see a doctor:
- cosmetic considerations;
- symptoms of discomfort;
- complications of the disease (for example, ulcers, bleeding or thrombophlebitis);
- fear for your health (how the disease will behave in the future if left untreated)
Sometimes it is difficult for a doctor to know what a patient wants. Therefore, during the consultation, it is important to find mutual understanding with the doctor, to correctly convey the main reason for his contact. Often patients simply need the belief that varicose veins will not harm them in any way and that they are unlikely to do so in the future.
If there is a need for therapy, the doctor often recommends undergoing self-medication at home within 6 months, which includes:
- use of compression stockings;
- regular exercise;
- avoid "long delays" - exclude long stays in a sitting or standing position;
- while resting (in a horizontal position), raise the "endangered" limb above the level of the heart.
If after the second consultation the patient is not satisfied with the result, the doctor may recommend conservative or surgical treatment of varicose veins of the lower extremities.
Possibilities of treatment of lower limb pathology
Conservative treatment (compression and pharmacological therapy, lifestyle changes), surgical interventions, external and internal laser exposure, radiofrequency ablation, injection sclerotherapy are used to combat varicose veins of the legs. The choice of this or that option depends on the patient's preferences. This is also influenced by the financial possibilities of the patients, the qualifications of the doctors and the equipment of the medical institution. However, which method of treating varicose veins of the lower extremities will be used in each case largely depends on the disease itself: what symptoms are present, the degree of venous insufficiency and other characteristics of vascular lesions.
Conservative methods of treatment
Conservative treatment is generally complex and involves several components.
Lifestyle change, which involves a set of measures aimed at preventing blood stagnation in the veins. As you know, prolonged standing or sitting position reduces the activity of the venous-muscular pump (gastrocnemius muscle), which contributes to stagnation. Therefore, patients are recommended to walk regularly, occasionally raising their legs above the level of the heart in a prone position. You should also pay attention to a variety of diet-salt-free, low-calorie. They will allow you to adjust your body weight, compensate for the seasonal lack of vitamins. It is necessary to consume foods rich in bioflavonoids (substances that help strengthen the walls of blood vessels).
People with varicose veins should avoid overheating their feet, refrain from visiting baths and saunas, and, if possible, do not use heated floors.
Compression stockings improve venous hemodynamics, which leads to the disappearance of many manifestations of the disease. Disadvantages of this method:
- limited use on time (there is no possibility of wearing compression stockings and socks all the time);
- the appearance of discomfort with constant compression, this is especially often observed in summer, when the symptoms of varicose veins are most "manifested".
The pharmacy usually offers compression stockings from only one manufacturer. However, there are many different brands, each of which can meet the needs of patients to a different extent.
Drug treatment can eliminate the symptoms of the disease or reduce their manifestation, is aimed at preventing and suppressing its complications, and can increase the effectiveness of compression therapy. Pharmacology helps to cope with the side effects that occur after sclerotherapy or phlebectomy.
Modern treatment of varicose veins of the lower extremities is not complete without the use of venotonics (phleboprotectors), drugs that can improve symptoms, strengthen the venous wall. They are considered basic pharmacotherapeutic agents. This includes:
- Wild chestnut fruit extract and thiamine (vitamin B1) are part of medications used to treat pain and heaviness in the legs, edema observed in chronic venous insufficiency. The drugs have shown their effectiveness in clinical trials. There are dosage forms: oral solution (10-15 drops 3 times a day) and tablet form (usually taken after a meal 1 tablet 3 times a day).
- Butcher's broom (butcher's broom) is used as a food supplement. Helps relieve venous congestion. It is believed to be effective against varicose veins. However, no clinical data have been established to confirm its safety and efficacy.
- Deproteinized hemoderivative of blood of young calves is part of popular drugs, which are excellent phleboprotectors, have a good therapeutic effect in varicose veins of the lower extremities.
As a rule, venotonics are prescribed in courses. The duration of the course depends on the dynamics of improvement of symptoms, the duration of remission achieved. Therefore, your doctor may change your medication intake from 3 to 6 months or more.
Ointments and gels (topical medications) are also widely used. The treatment regimen for varicose veins of the lower extremities is chosen by the doctor depending on the condition and course of the disease. The therapeutic effect of these topical drugs is realized through two mechanisms: disruptive and actually therapeutic. In the first case, the alcohol base or essential oils contained in the gel evaporate, which leads to a decrease in skin temperature, ie improves the symptoms of the disease. As a result of the second, the medicinal substance that has penetrated the skin directly into the vein begins to exert its therapeutic effect.
Ointments and gels used for varicose veins of the legs are classified according to the main active ingredient they contain. These include such medicinal substances:
- Phleboprotectors (usually rutin, as well as herbal substances that strengthen the vessel wall).
- Nonsteroidal anti-inflammatory drugs are commonly used to relieve pain.
- Topical corticosteroids are used for allergic dermatitis, which can occur as a complication of venous insufficiency.
- H1-histamine receptor blockers are prescribed instead of corticosteroids when these others are contraindicated.
- Proteolytic enzymes can effectively clear a trophic ulcer (complications of far-reaching varicose veins of the legs).
- Ionized silver is an effective antiseptic, perfectly cleanses and dries the wound, so it is an indispensable medicine for the treatment of infected trophic ulcer.
- Antibiotics are used topically for infections of varicose vein complications (thrombophlebitis, dermatitis).
- Rehydration preparations and dermatoprotectors protect the skin from external influences, improve its elasticity. They are usually prescribed for atrophic skin changes (when compression stockings are used for a long time).
- Heparin, in addition to antithrombotic action (prevents the formation of blood clots), also has an anti-inflammatory effect, can relieve pain.
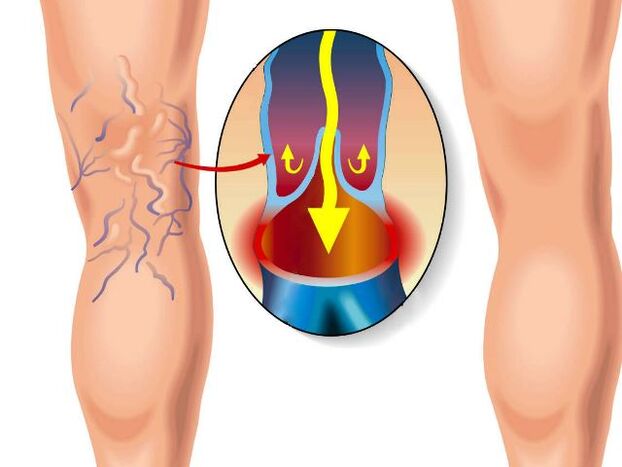
Surgery
The main goal of surgical treatment is to remove the pathological mechanism that led to the appearance of the disease - the venous reflex, as well as to remove its main manifestation - varicose veins. Surgical treatment is indicated: for patients with painful pain and constant fatigue in the legs, in the presence of edema, chronic venous insufficiency, cosmetic problems, early hyperpigmentation (excessive deposition of pigment in the skin), external bleeding, as well as in superficial thrombophlebitiswhich cannot be treated by conservative methods.
Currently, the three most popular types of surgery are:
- sapheno-femoral ligation (ligation and removal of the upper part of the great saphenous vein);
- striated large saphenous veins:
- traditional or Bebcock surgery, in which a special probe is inserted into the lumen of a large subcutaneous vein (previously two incisions were made: one in the groin area, the other at the level of the upper third of the leg) and extends along its entire length, after which it is removed along with the dilatedvenom;
- cryostripping, an operation that is almost similar to the previous one, but differs in that the probe is cooled to -85 ° C, due to which the vein sticks to the probe, which allows for less traumatic removal;
- Phlebectomy is a procedure to remove varicose veins through several small, 2-3 mm incisions in the skin.
The above surgical interventions help to improve the quality of life of the patient; their therapeutic and economic efficacy has been proven in clinical trials. They are usually performed under general anesthesia, but most patients are discharged on the day of surgery. Complete recovery, return to normal daily activities usually takes 2 to 3 weeks. Complications are possible, which are more common in patients with advanced varicose veins. During the operation, the nerves located in the subcutaneous tissue can be damaged, so after surgical manipulation, temporary or even permanent numbness of some parts of the legs is sometimes noticed, but this does not lead to serious disability.
New treatments
The main goal of using new treatment methods is to minimize the tissue trauma observed during surgical interventions, allowing the patient to recover faster. They began to be widely used in the early 2000s.
Intravenous ablation (RF and laser)
Radiofrequency and laser ablation are methods of treating varicose veins of the legs by "sealing" the great saphenous vein (or small) at high temperature, which leads to regression of the dilated veins (their walls are held together). Although these options do not include surgery, it is quite common to resort to additional phlebectomy and sclerotherapy. Both methods include:
- Catheter insertion into the great saphenous vein through a small incision in the upper third of the leg and progressing to the saphenofemoral joint under ultrasound supervision. No incisions are made in the groin area.
- Performed under local anesthesia (the anesthetic is intensively infiltrated into the subcutaneous tissue of the upper leg). Additional general anesthesia may be required if a large number of miniphlebectomies are to be performed simultaneously.
- The need to use bandages or socks after the procedure for two weeks.
- The dependence of their result on the anatomy of the saphenous veins in the patient is positive in the presence of straight lines, suspicious when the veins are curved.
The use of intravenous ablation, which has been widely used in the last ten years, has not shown significant differences in its efficacy compared to surgery.
The main advantage of this technique is fast recovery after the procedure, which is associated with a lower probability of wound infection and the appearance of hematomas.
However, complications are typical for this procedure: skin burns, temporary paresthesias, deep vein thrombosis (occurs in less than 1% of patients).
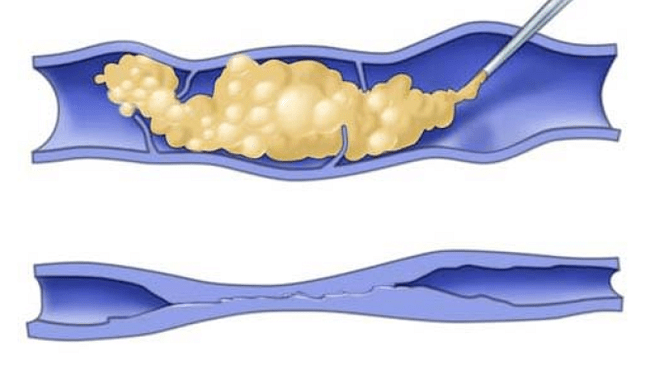
Simple sclerotherapy
This method of treatment, due to the simplicity of implementation and low trauma, is currently used by many clinics. Its essence lies in the fact that sclerosant is injected into varicose veins, substances that stick to its walls, and blood flow passes into healthy blood vessels. Sclerotherapy is often combined with classic operations, and in the case of telangiectasia and spider veins, it is used as the only method of therapy.
Contraindications:
- pregnancy,
- breastfeeding period,
- dermatitis,
- thrombophlebitis.
Sclerotherapy gives quite acceptable results that satisfy many patients.
Foam sclerotherapy
Unlike simple sclerotherapy, with foam, sclerosant is injected into a vein after mixing with gas (usually air). As a result, foam is obtained which, spreading through the vein, squeezes the blood out of it and causes the vessels to spasm. Usually the manipulation is performed under the guidance of a duplex ultrasound scan.
In addition to simple foam sclerotherapy, it is necessary to wear compression stockings for 14 days.
Recovery after the procedure is faster than if a classic operation was performed. However, the medium-term treatment outcomes (likelihood of recurrence of reflux) of sclerotherapy with foam are somewhat worse than those after surgery.
Treatment of "microvaricosis": telangiectasia, spider veins
Treatment of spider veins is almost always carried out only for cosmetic reasons, although sometimes they can cause a hot, pulsating sensation, indicating the presence of reflux. Two types of therapy are usually used:
- Microsclerotherapy - introduction of a sclerosing substance using a thin needle. Usually several spider veins are sclerosed at the same time. A compression bandage or sock is applied for 1 to 2 days. If sclerosis comes out of the vessel during injection, an ulceration may develop in the area that heals slowly, leaving a scar. This rarely happens, provided "if the doctor’s hands don’t shake during surgery". Hyperpigmentation at the injection site (darkening of the skin) is also possible.
- Laser ablation. The method works well for the treatment of telangiectasia (intradermal vascular growth that looks like a birthmark).
There are many effective ways to remove varicose veins of the lower extremities offered by traditional medicine. The choice of treatment largely depends on the decision of the patient. Don't "go under the knife" right away, there are effective possibilities for conservative therapy in the doctor's arsenal. According to doctors, today it is impossible to completely cure this disease, but it is quite within the capabilities of modern medicine to save the patient as much as possible from the manifestations of the disease and prevent its further progression.




































